What’s Lurking in the Dust? (Black Lung Disease Part 2: Drug Therapy)
Summary:
Black lung disease (CWP) has no cure, but management relies on bronchodilators, corticosteroids, oxygen therapy, and—at end-stage—lung transplantation. Pulmonary rehab and prevention add value but drug regimens can quickly escalate in cost and complexity. For payers, early oversight and structured monitoring are critical—to prevent duplicate fills, mitigate steroid side effects, and manage high-cost interventions like oxygen and transplant. Prodigy ensures therapy is clinically appropriate, financially defensible, and aligned with patient outcomes.
Managing Coal Workers’ Pneumoconiosis with Clinical and Claims Oversight
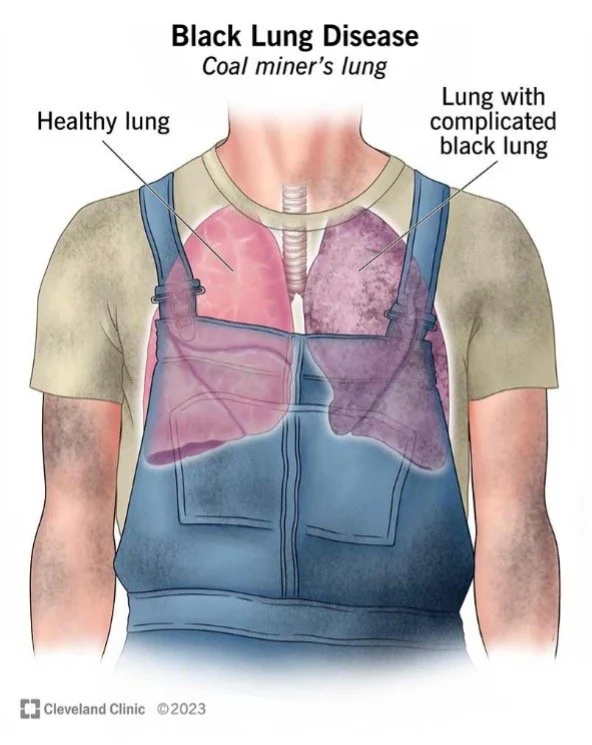
In our earlier feature, “What’s Lurking in the Dust?”, we explored the long-term risks of coal dust exposure and the rise of coal workers’ pneumoconiosis (CWP), better known as black lung disease. This follow-up turns to the treatment landscape—what medications are being used, how they work, and why payer oversight is essential. While there is still no cure, drug therapy and supportive care play a vital role in slowing progression, relieving symptoms, and improving quality of life for affected workers .
For payers, these regimens can be complex and costly. Overlapping conditions like COPD and emphysema increase drug utilization, while long-term oxygen therapy or transplant evaluations add additional layers of expense. This is where proactive review, monitoring, and structured intervention become critical.
Pulmonary Rehabilitation – A Non-Drug Foundation
Before medications even enter the picture, pulmonary rehab is the cornerstone of care. Programs combine breathing techniques, graded exercise, endurance building, nutrition education, and mental health support. Structured courses typically last about eight weeks and can meaningfully improve symptom control . For payers, these programs represent a lower-cost, high-value investment—reducing exacerbations and downstream spend on emergency interventions.
Drug Therapies in Focus
1. Bronchodilators
Bronchodilators are often the first line for symptomatic patients, especially those with COPD overlap.
Short-acting beta-2 agonists (SABAs) such as albuterol or levalbuterol provide rapid relief during flare-ups.
Long-acting beta-2 agonists (LABAs) like salmeterol or formoterol, and anticholinergics such as ipratropium (short-acting) and tiotropium or aclidinium (long-acting), provide sustained bronchodilation .
Clinical guidelines recommend combination therapy for persistent symptoms. Evidence shows bronchodilators improve lung function, reduce dyspnea, and enhance exercise tolerance in CWP with obstructive features . For payers, these agents highlight the importance of formularies, step-therapy logic, and refill monitoring—to ensure appropriate use without duplication.
2. Corticosteroids
Oral corticosteroids reduce inflammation but bring heavy side-effect risks: fluid retention, glucose shifts, hypertension, infection risk, mood swings, and ocular issues such as cataracts . Inhaled corticosteroids (budesonide, mometasone) offer localized action with fewer systemic effects .
For payers, corticosteroid therapy requires clinical guardrails—balancing symptom relief against long-term cost drivers like steroid-induced diabetes or hospitalizations from infection.
3. Oxygen Therapy
As fibrosis worsens, patients develop hypoxemia—low oxygen saturation that stresses the heart and brain. Supplemental oxygen becomes essential at this stage . While life-sustaining, oxygen therapy also represents a major recurring cost, particularly in rural or at-home settings.
4. Lung Transplantation
For end-stage disease, lung transplantation may be considered. Since the first CWP transplant in 1996, outcomes have proven comparable to other advanced lung diseases . Despite severe baseline features (pulmonary hypertension, dialysis risk, ECMO use), transplant survival is not significantly worse .
From a payer perspective, transplant is rare but high-cost—underscoring the need for early intervention upstream to reduce progression to this point.
Prevention Still Matters
Even with drug therapy, prevention remains critical:
Smoking cessation and avoidance of secondhand smoke.
Limiting dust and silica exposure; tracking daily air quality .
Annual influenza and pneumococcal vaccination .
Regular activity with caution against overexertion.
Symptom tracking and early reporting for timely intervention.
Each prevention step reduces downstream claims exposure and keeps patients more stable in the community.
Prodigy’s Perspective: Why Oversight Counts
For payers, black lung disease highlights why clinical oversight of drug therapy isn’t optional. At Prodigy, we view occupational diseases like CWP through a dual lens: patient outcomes and payer protection.Careful monitoring, prior authorization, and proactive reviews prevent unnecessary costs while ensuring workers receive the right therapy at the right time. That balance—clinical precision with financial stewardship—is the path forward in managing black lung disease.
By Ashley Lozano
PharmD Candidate (P4)
For questions, e-mail pharmd@prodigyrx.com
Citations